A Brief History of Endotracheal Intubation

In modern medical practice the establishment of a safe, secure airway has become a mainstay of anaesthesia and critical care medicine. We work in an increasingly technological age of medicine, and airway management has unsurprisingly followed suit. The use fiber-optics and advanced video imaging techniques to visualize the larynx and attempt to relieve or prevent airway obstruction are becoming more common. Yet it may come as a surprise to course participants to learn how far back in history our medical predecessors have been trying to deal with this challenge.
Earliest evidence of airway management is of tracheotomy. Symbols describing this procedure have been found on Egyptian tablets that are dated to around 3600BC and later in the Eber’s Papyrus, written in Thebes around 1500BC, currently held in the University of Leipzig. [1] This 20-meter-long scroll also describes the treatment of Guinea-Worm infection, which remains the standard today. Apart from this and tracheotomy, most of its other remedies are best not applied to modern medical practice. There are references to tracheotomy in one of the ancient Hindu scripture texts, The Rigveda, also composed around 1500BC.
The Greeks had a lot to say about tracheotomy, much of which was not encouraging. Hippocrates (of the eponymous Oath, 450-370BC) felt the risks of carotid arterial laceration and poor healing of fistulas were excessive and condemned the procedure as too dangerous. [2] A few reporters were more favorable, including Galen (129-199AD) and Antyllus, who described a horizontal incision like the modern technique. More sensationally, Homerus of Byzantium documented the story of Alexander the Great performing a tracheotomy with his dagger point to save one of his troops from asphyxiation. The soldier was said to be choking, on what we are uncertain, and the long-term outcome is also unsure. [3]
While most of Europe descended into the Medieval Dark Ages, with little scientific exploration, elsewhere in Persia and Islamic Iberia surgical advances continued. Descriptions emerged of tracheal wound healing after repair and clarification of the anatomy of the trachea by physicians such as Ibn Zuhr. However it was only much later, in 1546 that Brassavola of Ferrara described a successful tracheostomy. This was used to treat a patient with peritonsillar abscess who made a full recovery, the first recorded occurrence. Unfortunately mortality remained high during tracheostomy and it became a last ditch procedure in patients close to death from airway obstruction.
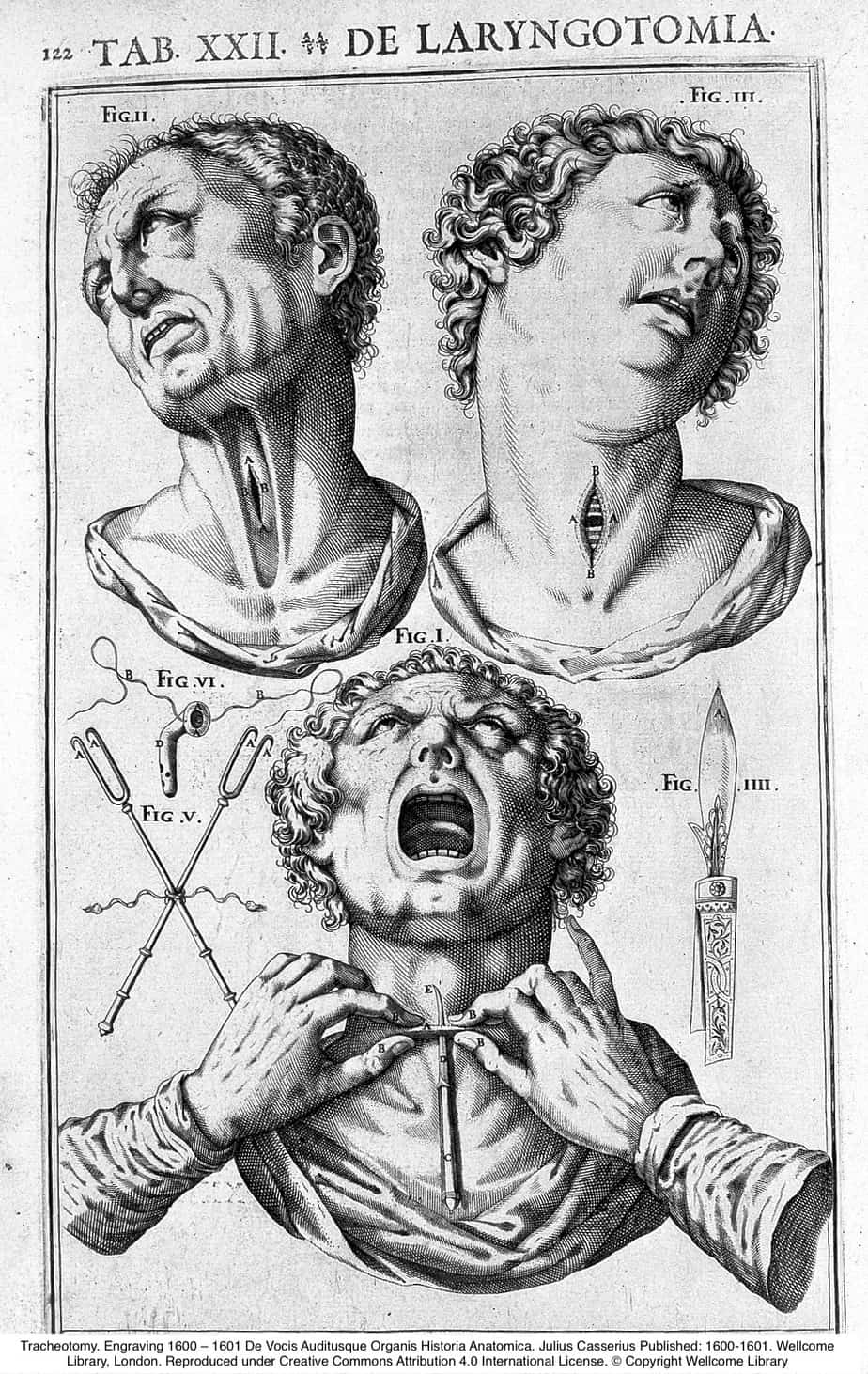
As is often the case, procedures improved out of necessity, and during diphtheria outbreaks in Europe during the mid 19thCentury, tracheostomy became an established treatment for acute airway obstruction following the work of Armand Trousseau (1801-67). Later in the 1870’s Friedrich Trendelenberg (1844-1924) performed tracheostomy electively for a patient undergoing oral surgery under early general anaesthesia. The introduction of a cannula or tube to the trachea reduced the risk of blood aspiration. The procedure was further refined by Chevalier Jackson (1865-1958) in Philadelphia in the early 20thcentury and remains a standard to this day.
Even before the tracheostomy procedure became well established in the 19thCentury attempts were made to provide non-surgical solutions to airway management. During the 18thCentury attempts at artificial respiration using bellows inserted into the mouth were often attempted for patients in near drowning episodes. In 1788, Charles Kite, a Surgeon working in London, described the use of a curved narrow metal catheter inserted into the larynx via the nostril in a blind technique, which then could be used to apply ‘bellows’ respiration.’ Interestingly this also had an attachment to block off the oesophagus and prevent the tongue falling back. He outlined this in his paper “An Essay on the Recovery of the Apparently Dead” [4] and is thought to be the first description of an endotracheal intubation. In France a similar catheter techniques were attempted, but fell out of use due to over vigorous bellows ventilation leading to ‘emphysema’ or more likely pneumothorax.
Airway obstruction due to diphtheria pseudomembranous disease was also the stimulus to explore non-surgical tracheal intubation. Eugene Bouchet (1818-91), a Paediatrician in Paris, explored a procedure to introduce a short silver tube into the larynx to relieve airway obstruction due to diphtheria. The tube was secured with a silk thread to prevent it moving to far in, and was to be removed after several days when the obstruction was relieved. The patient was awake during the procedure and the tubes were of one size only. Bouchet presented 7 cases to the French Academy of Sciences in 1850 and was roundly condemmed, particularly by Armand Trousseu who as we know was an advocate of tracheostomy at the same time. Of Bouchet’s 7 cases, only 2 survived and both required tracheostomies subsequently. He still persevered and Bouchet’s tubes became an alternative to tracheostomy.
Other proponents were William McEwan (1848-1924), a Scottish surgeon who performed blind endotracheal intubation on patients with laryngeal oedema and also to administer chloroform for anaesthesia during oral surgery. [5] In the USA, Joseph O’Dwyer, a New York Paediatrician, advanced Bouchet’s work with a metal tube to relieve diphtheria airway obstruction, producing a set of varying sized tubes for greater comfort and an introducer system to aid the blind technique.

A lot of assistance was also needed from one of the parents, and the technique involved the operator’s fingers being inserted into the mouth of the child, which risked biting and subsequent infection to the doctor! However this became a life saving technique until the introduction of a diphtheria vaccine in the early 20thcentury.
These early efforts were plagued by significant failure rates due to being ‘blind’ techniques and were difficult to teach, although O’Dwyer towards the end of his career claimed he never failed to intubate the trachea. As anaesthetic agents improved interest gathered in using endotracheal intubation to administer volatile agents rather than relying on mask techniques, following on from McEwan’s work. The added benefit of protecting the airway from soiling during oral surgery and reducing the risk of aspiration was also considered. Among the many scientific advances in the 19thCentury, the science and techniques of optics improved dramatically, with the introduction of many instruments with medical applications and the ‘birth’ of endoscopy. It is remarkable how many body cavities were accessible by metallic tubes with mirrors and early light sources (sometimes candles!) Laryngoscopy had previously been performed indirectly with mirrors, but in 1895 Albert Kirsten (1863-1922) performed the first direct laryngoscopy in Berlin, using his ‘Autoscope’. This was in fact a modified rigid oesophagogastroscope. He was inspired to this development having heard reports of accidental tracheal visualization during oesophagoscopy. The device was bulky however and had a detachable light source on its handle. The idea was improved on by Chevalier Jackson (of tracheostomy fame) in 1913, who produced a device with a distal light source to visualize and intubate the trachea. Part of the blade had to be removed to allow the passage of a tube or a bronchoscope. Henry Janeway in the same year produced a device that ran on batteries, with a narrower curved blade, and was intended solely for intubation of the trachea, further improving the concept. His laryngoscope would not look out of place on a modern anaesthetic trolley. Sir Robert McIntosh’s curved and Miller’s straight laryngoscope blades were introduced in the 1940’s and these are in fact found still on modern anaesthetic trolleys. McIntosh is also credited with the first use of a Gum elastic bougie as an introducer for an endotracheal tube.
Intubation had become a routine procedure in Europe during the period between World Wars, but in the USA it was not as commonplace. At this time Aurthur Guedel began work with larger bore rubber tubes that also allowed exhaust gas flow i.e. permitted ventilation and also with an inflatable cuff that was positioned just distal to the vocal cords, to prevent soiling of the airway. He advocated intubation by travelling around the USA with his ‘Dunking Dog Show’ during which he would anaesthetize his pet dog called Airway (yes, really), and following intubation would immerse the poor pooch in a water bath and ventilate the lungs. The dog would then emerge intact from anaesthesia and the water bath, and would run off the stage, not surprisingly!
With the onset of World War II, the need for early trauma surgery in the field led to increased proficiency with airway techniques. This coincided with the development of neuromuscular blockade using curare by Harold Griffiths and Enid Johnson in 1942. This used in combination with volatile hypnotic agents allowed the patient to be sedated and paralysed for intubation and surgery. The practice of modern airway management in anaesthesia and critical care medicine has grown from these developments.
Interestingly today we are returning to some historical techniques but with a modern twist. Sedating and paralyzing patients is not always the safest way to proceed, particularly in cases with airway obstructing pathology. Awake intubation was previously noted to be traumatic for the patient and for the doctor as some of O’Dwyers’s students found out. Today thin flexible fiberoptic scopes used in conjunction with topical local anaesthesia have reintroduced the practice of awake intubation, although this is not common in paediatric practice. Additionally indirect laryngoscopy has re-emerged with the development of videolaryngoscopes eg. Glidescope, Airtraq and C-MAC. The larynx is visualized by either a camera lens at the tip of the device or via internal prisms reflecting into a proximal camera. These devices may improve success safety of intubation where difficulty may have previously been encountered, but introduce a new range of skills that differ from those of traditional direct laryngoscopy. It could be said that these advances show as we move forward it is sometimes worthwhile looking over one’s shoulder to what has past for inspiration.
References
- Pahor, Ahmes L. (2007). “Ear, Nose and Throat in Ancient Egypt”. The Journal of Laryngology & Otology. 106(8): 677-87.
- Jones, W. H. S. (2009). “Hippocrates in English”. The Classical Review. 2(2): 88-9.
- Szmuk, Peter; Ezri, Tiberiu; Evron, Shmuel; Roth, Yehudah; Katz, Jeffrey (2007). “A brief history of tracheostomy and tracheal intubation, from the Bronze Age to the Space Age”. Intensive Care Medicine. 34(2): 222-8.
- Kite, Charles (1788) “An essay on the Recovery of the apparently dead”. Dilly- London. Now held in Leads University Library Archive.
- MacEwen, W. (1880). “Clinical Observations on the Introduction of Tracheal Tubes by the Mouth, Instead of Performing Tracheotomy or Laryngotomy”. BMJ. 2(1022): 163-5.
![]()