Paediatric Airway Anatomy
A clear understanding of the clinical anatomy of the paediatric airway is essential when
- Appropriately positioning children undergoing intubation
- Interpreting structures seen on direct laryngoscopy
- Selecting the correct equipment for intubation
Laryngeal Anatomy
The larynx is the key anatomical structure that needs to be identified when carrying out intubation. The larynx is a cartilaginous structure slung from the hyoid bone by the hyothyroid membrane. It comprises of numerous separate cartilages held together with connective tissue.
The ligaments of the larynx (antero-lateral view). Gray H. Anatomy of the Human Body, 1918. Reproduced with kind permission of Bartleby.com
Anteriorly the large shield like thyroid cartilage lies deep to the thyroid gland and the prominence of which forms the Adam’s apple in men. Inferior to this cartilage lies the cricoid cartilage which is signet ring shaped and completely encircles the airway. Between these two structures the connective tissue condenses to form the cricothyroid membrane (a key structure for front of neck access).
The ligaments of the larynx (posterior view). Gray H. Anatomy of the Human Body, 1918. Reproduced with kind permission of Bartleby.com
Posteriorly the epiglottis, a leaf shaped cartilage, projects superiorly. Lying above the cricoid cartilage posteriorly are the 2 pyramidal arytenoid cartilages. Projecting from the anterior point of the arytenoid cartilages are dense condensations of avascular connective tissue that form the true vocal cords.

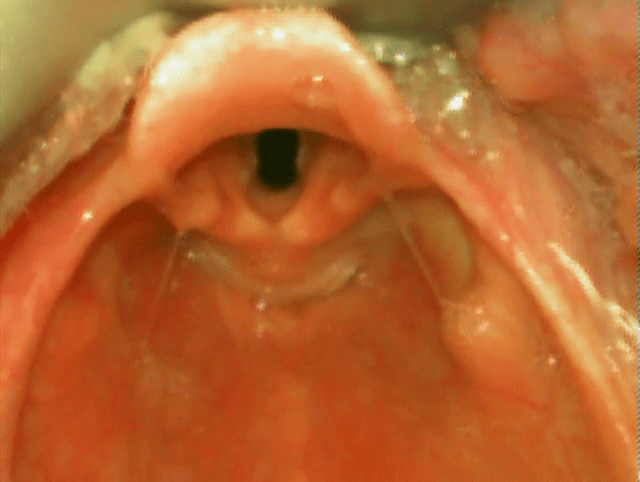
Superior view of larynx on laryngoscopy
When carrying out laryngoscopy these structures are viewed from above. From this perspective the leaf shaped epiglottis lies anteriorly, projects superiorly and appears omega shaped. Anterior to the epiglottis is the vallecula, which contains the glossoepiglottic ligament connecting the base of the tongue to the epiglottis. The arytenoid cartilages are seen as two swellings posterior to the epiglottis. Between these structures the avascular (white) true vocal cords with the midline tracheal opening can be seen.
The oesophagus lies posterior and inferior to the laryngeal inlet. This close proximity explains the frequent propensity for the uninitiated to misplace an endotracheal tube (ETT) resulting in oesophageal intubation. This should be avoidable if time is taken to correctly identify key laryngeal structures prior to placing the ETT.
The airway view can be graded based on how clearly these structures can be visualised. A commonly used grading scheme is the Cormack-Lehane classification system detailed below.
Cormack-Lehane classification system
Grade 1
Complete view of laryngeal inlet

Grade 2
Partial view of laryngeal inlet, subdivided into:
2a
Partial view of vocal cords

2b
Arytenoids visible but no view of vocal cords

Grade 3
Epiglottis only visible

Grade 4
No laryngeal structures visible

The larynx and upper airways receive sensory innervation from the vagus nerve. Stimulation in this region can result in high vagal tone resulting in bradycardia. This reflex is particularly pronounced in neonates and can be addressed pharmacologically if required (Intubation Pharmacology). Motor innervation is via the recurrent laryngeal nerve. Damage to this nerve results in vocal cord paralysis.
The larynx can be divided into a supraglottic compartment above the vocal cords and the subglottic space below. The supraglottic compartment is where supraglottic airways such as the laryngeal mask airway (LMA) are placed whilst damage to the subglottic space can result in subglottic stenosis, a potential complication of intubation.
Upper airway anatomy
In order to open the paediatric airway and gain the best view of the laryngeal inlet the oral, pharyngeal and tracheal axes must be brought into alignment. This requires suitable patient positioning during preparation for intubation and differs based on the age of the child.
In an older child the optimal position is the sniffing the morning air position where the child’s head and neck are extended and brought slightly anterior. Obtaining this position can be aided by placing a small towel below the child’s head.
However, in the infant this approach will only lead to excessive neck flexion due to the presence of a prominent occiput. In infants placing the babies head in the neutral position and bringing the body forward with the aid of a shoulder roll best aligns the axes.
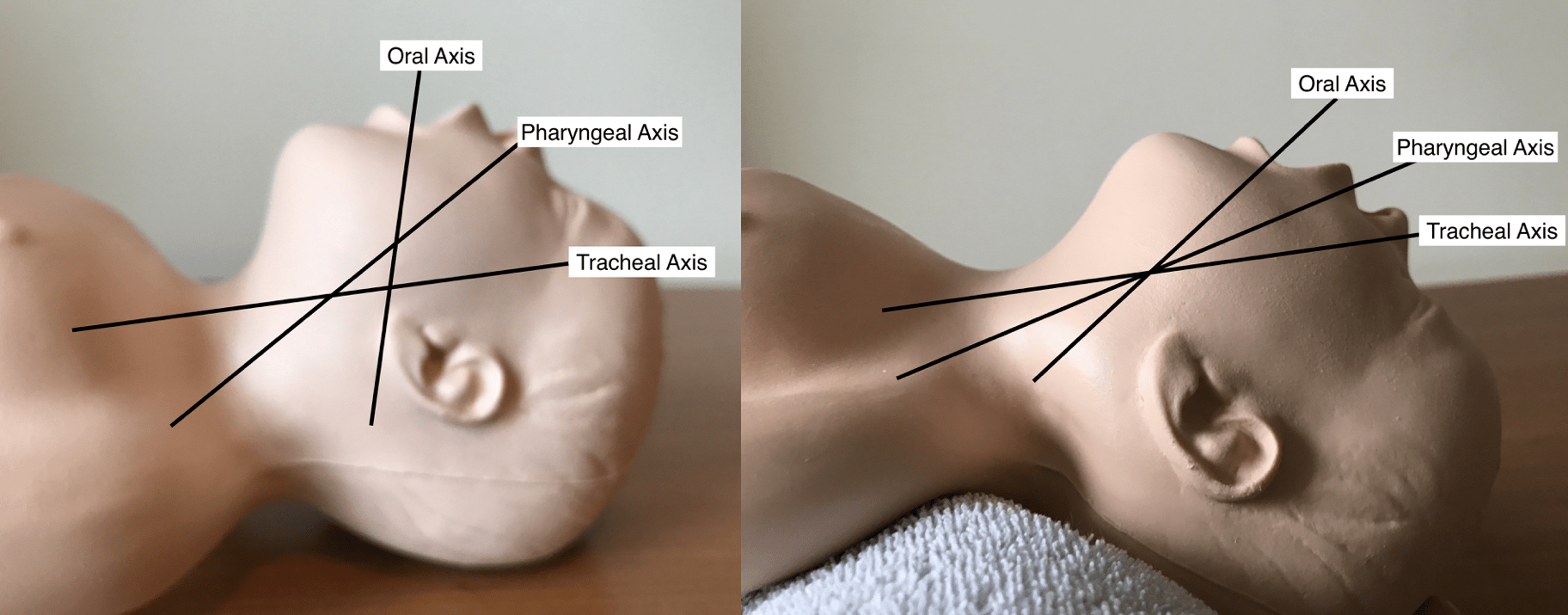
Alignment of oral, pharyngeal and tracheal axes by using a shoulder roll in a neonate

Demonstration of the ear to sternal notch positioning. Reproduced with kind permission of Dr Chris Thompson
The goal in both these situations is to bring the tragus of the ear and the sternal notch into horizontal alignment.
Anatomical differences
Children and not just small adults and their airway anatomy thus differs. These differences have a number of implications for intubation practice. As already mentioned optimal position differs for infants and children due to the presence of a prominent occiput in infants.
In infants the laryngeal opening is typically higher (C1 infancy, C3/4 childhood, C4/5 adulthood), the epiglottis is usually longer and floppier, and the glossoepiglottic ligament more lax than in older children. This has implications on which laryngoscope blade type you should select. The two most commonly used type of laryngoscope blades in children are straight blades e.g. Miller blade and curved blades e.g. MAC blade. The straight blade is designed to directly lift the epiglottis out of the way, while the curved blade is designed to indirectly lift the epiglottis by exerting pressure on the glossoepiglottic ligament it in the vallecula.
A straight blade is generally preferred in neonates and young infants as a combination of their high tracheal inlet position, large floppy epiglottis and laxity of the glossoepiglottic ligament in this age group often results in an incomplete laryngeal exposure when a curved blade is used. A curved blade is generally used from 6-12 months of age, however a straight blade can be used in all age groups depending on personal preference.
Finally, the paediatric airway is funnel shaped with narrowest point being the cricoid cartilage. In contrast, the adult airway is barrel shaped with narrowest point being the vocal cords. This fact has implications on the type and size of ETT that should be selected for intubation.
Endotracheal tube choice
The airway and laryngeal structure size varies in children with growth. This means that equipment must be sized according to the size of the child.
Traditionally children under the age of 8-10 years were intubated with uncuffed endotracheal tubes due to concerns about subglottic stenosis and cuffed tubes were only used in this age group in special circumstances such as burns and asthma. In these situations a seal was obtained by selecting an ETT that would fit snuggly within the cricoid cartilage and prevent leak via cricoid sealing. Sizing of the ETT was often calculated using formulae.
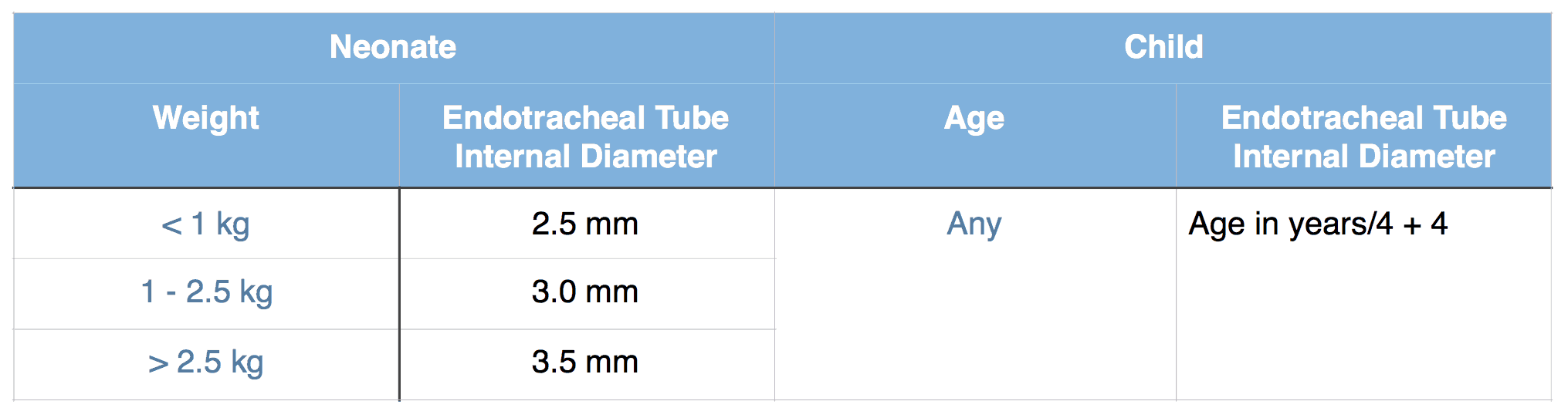
Uncuffed Endotracheal Tube Sizing
In recent years there has been a trend towards using cuffed endotracheal tubes routinely in all children due to the advantages of improved ventilation and a lower rate of reintubation due to leak from an uncuffed tube that is too small. Provided the cuffed tube is appropriately sized, its use isn’t contraindicated (preterm or weight < 3 kg) and cuff pressures are monitored, their use in children appears to be safe and is supported by major resuscitation guidelines. The Microcuff tube is the only currently available cuffed endotracheal tube specifically designed for the paediatric airway and has a number of advantages over the other traditional cuffed tubes (see podcast on Should cuffed endotracheal tubes be used routinely in critically ill children? for more details). For these reasons I would recommend that critically ill children are intubated with a Microcuff tube provided it isn’t contraindicated. Microcuff ETTs are sized based on manufacturer recommendations.
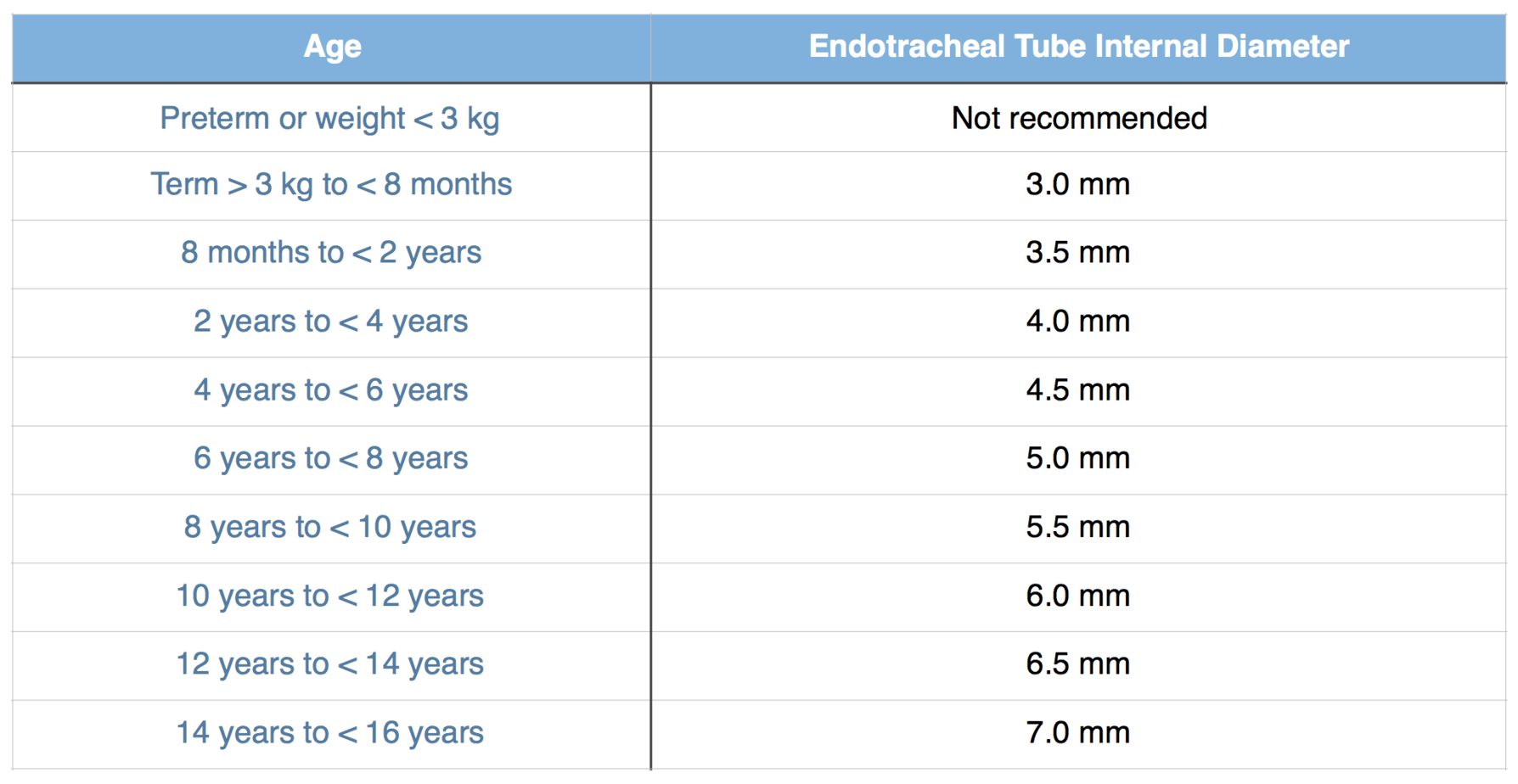
Microcuff Endotracheal Tube Sizing (manufacturers recommendations)
Endotracheal tubes have depth markers which are designed to be positioned at the level of the cords to aid correct positioning of the endotracheal tube in the mid trachea.

Depth marker on a Microcuff tube positioned at the level of the vocal cords
The accuracy of these depth markers in children varies widely between manufacturers with some being grossly inaccurate as the linked article demonstrates. It showed 15 brands of endotracheal tubes positioned at the mid trachea (MT) level demonstrating that many of the depth markers are far away from the glottic level (GL) line and what is more concerning is that many of the endotracheal cuff balloons lie at the level of the glottic opening where they could potentially cause damage to the vocal cords. This study demonstrated the need for an endotracheal tube that was specifically designed for the paediatric airway and so the Microcuff tube was developed. It is important you know the accuracy of the depth marking on the brand of endotracheal tubes you use and we would recommend using one where the marking have been shown to be accurate in children such as the Microcuff tube.
An alternative method to estimate how far to insert the endotracheal tube is to use one of the formulae below.
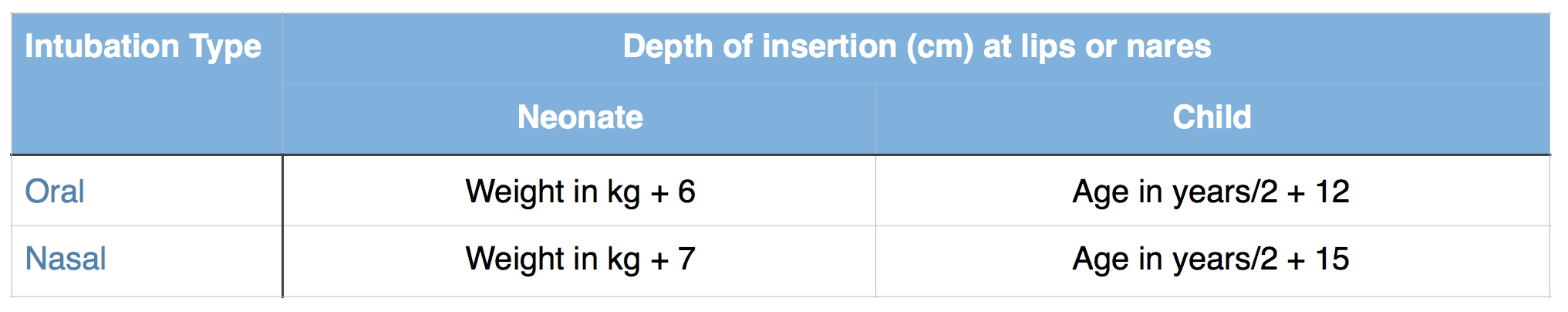
Formulae to estimate depth of insertion of endotracheal tube
No matter which method is used to estimate the depth of insertion this should be adjusted initially using auscultation (equal air entry bilaterally) and then by performing a chest radiograph (tube positioned midway between clavicles and carina).

Endotracheal tube correctly positioned below the clavicles and above the carina

Endotracheal tube positioned too high at level of clavicles

Endotracheal tube positioned too low in right main bronchus
![]()