LMA Insertion
History and use of the LMA
The laryngeal mask airway (LMA) is a very useful airway device and it has significantly changed airway management since it was first used in the late 1980s. On the one hand, it has given opportunities to use a less invasive and easier to place airway than a tracheal tube, and, on the other hand, allowed the practitioner to be freed up to do other tasks when compared with the use of the face mask. It is an excellent addition to the difficult airway trolley. However, the LMA needs to be used wisely, especially when it is used where there may be indications for using a tracheal tube.
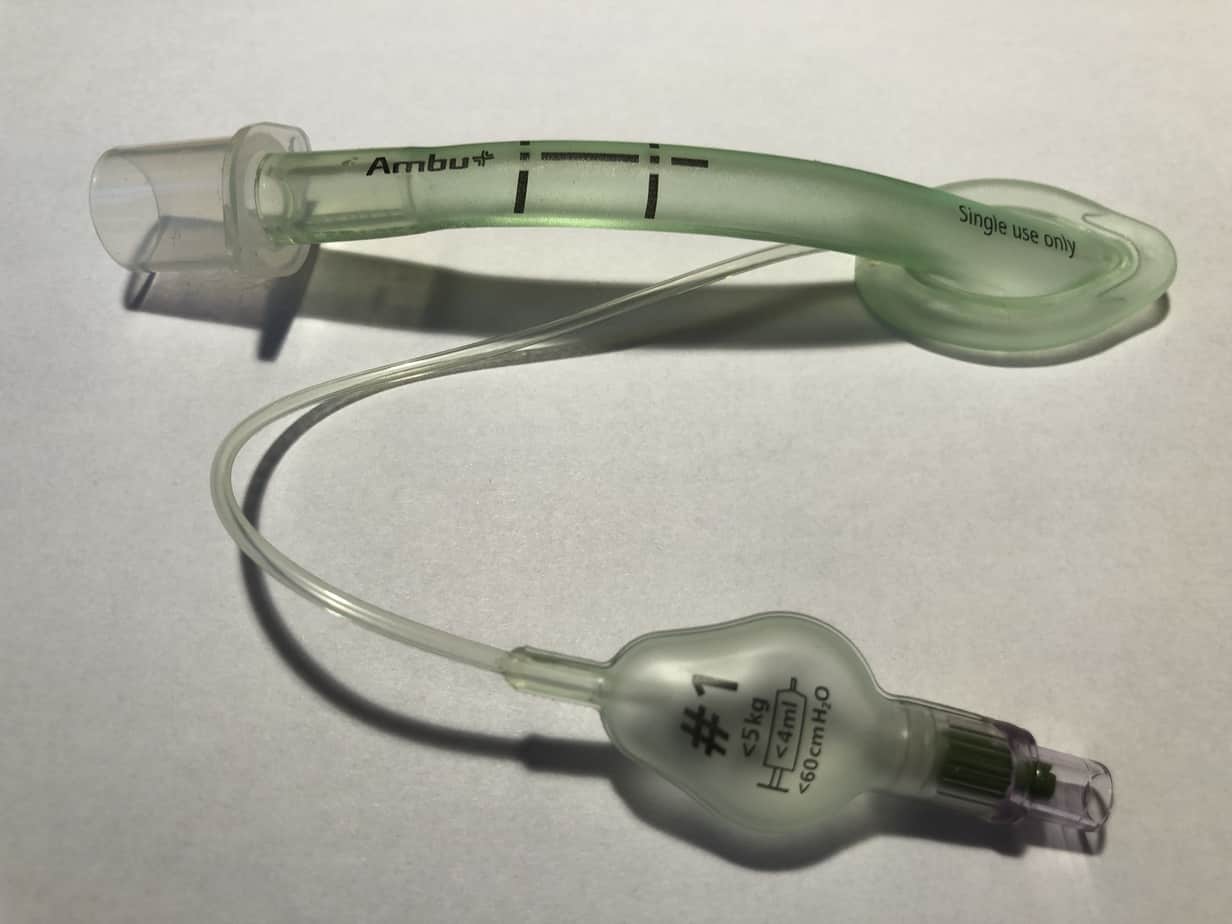
The LMA is a type of supraglottic airway, which comprise a tube whose distal end is connected to a large elliptical mask with a cuff. The ‘first generation’ LMA has been modified in various ways in order to offer improvements, and flexible LMAs, proseal LMAs, and iGELs are probably the most common variants.
The LMA was perhaps first designed for spontaneously breathing patients, but it has proven itself to be safe and useful in certain situations for patients who require controlled ventilation.
Its use has also become firmly established in the management of the difficult airway. In a ‘can’t ventilate’ situation, it often provides a clear airway where it was impossible to establish one using a facemask alone, and in a ‘can’t intubate’ situation, it can provide a temporary airway which allows ventilation and a conduit for intubation.
Insertion of LMA
Insertion of an LMA is a skill which is quickly learned, although regular and sustained clinical practice using LMAs will help significantly in difficult situations.
The following technique is that as originally described:
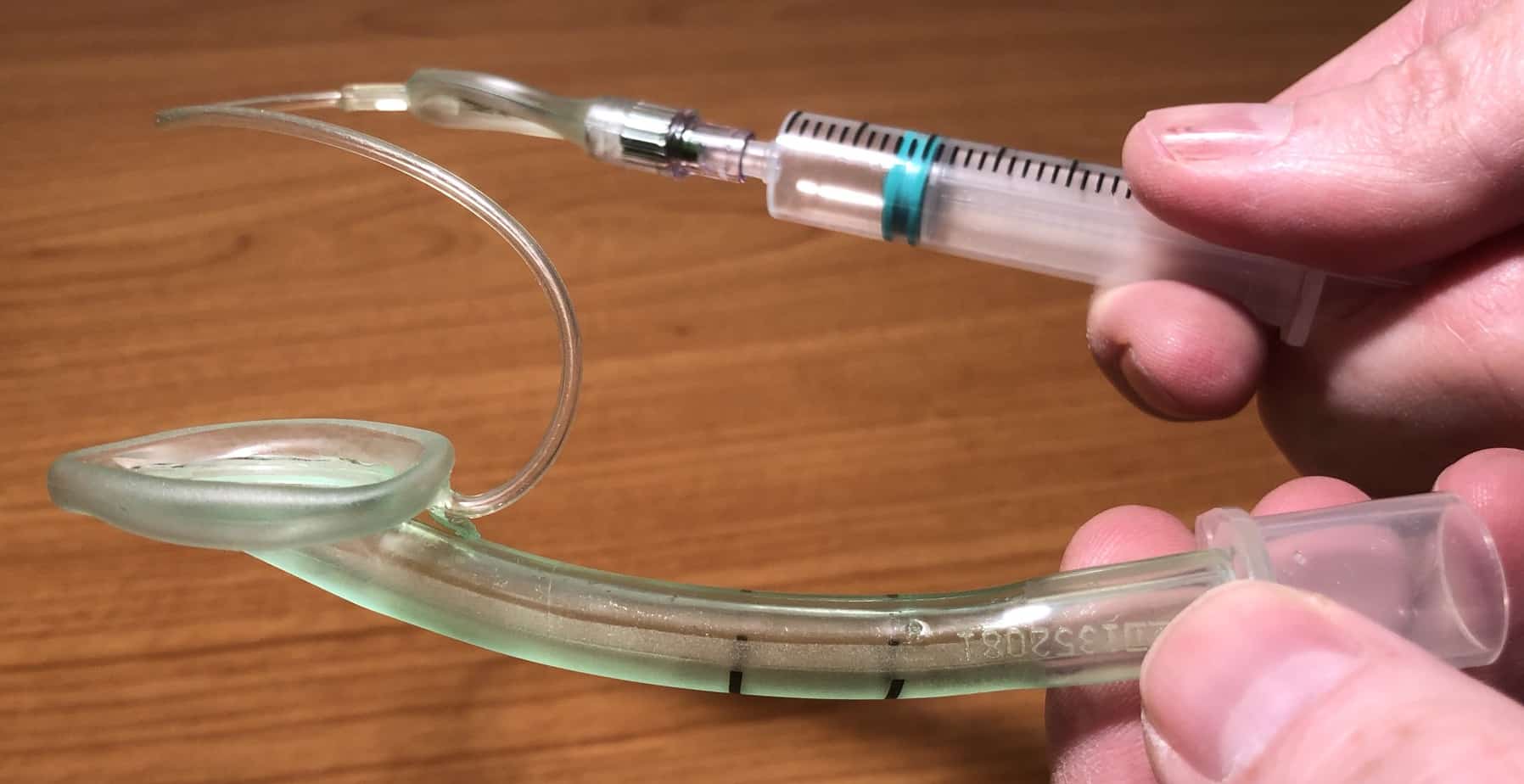
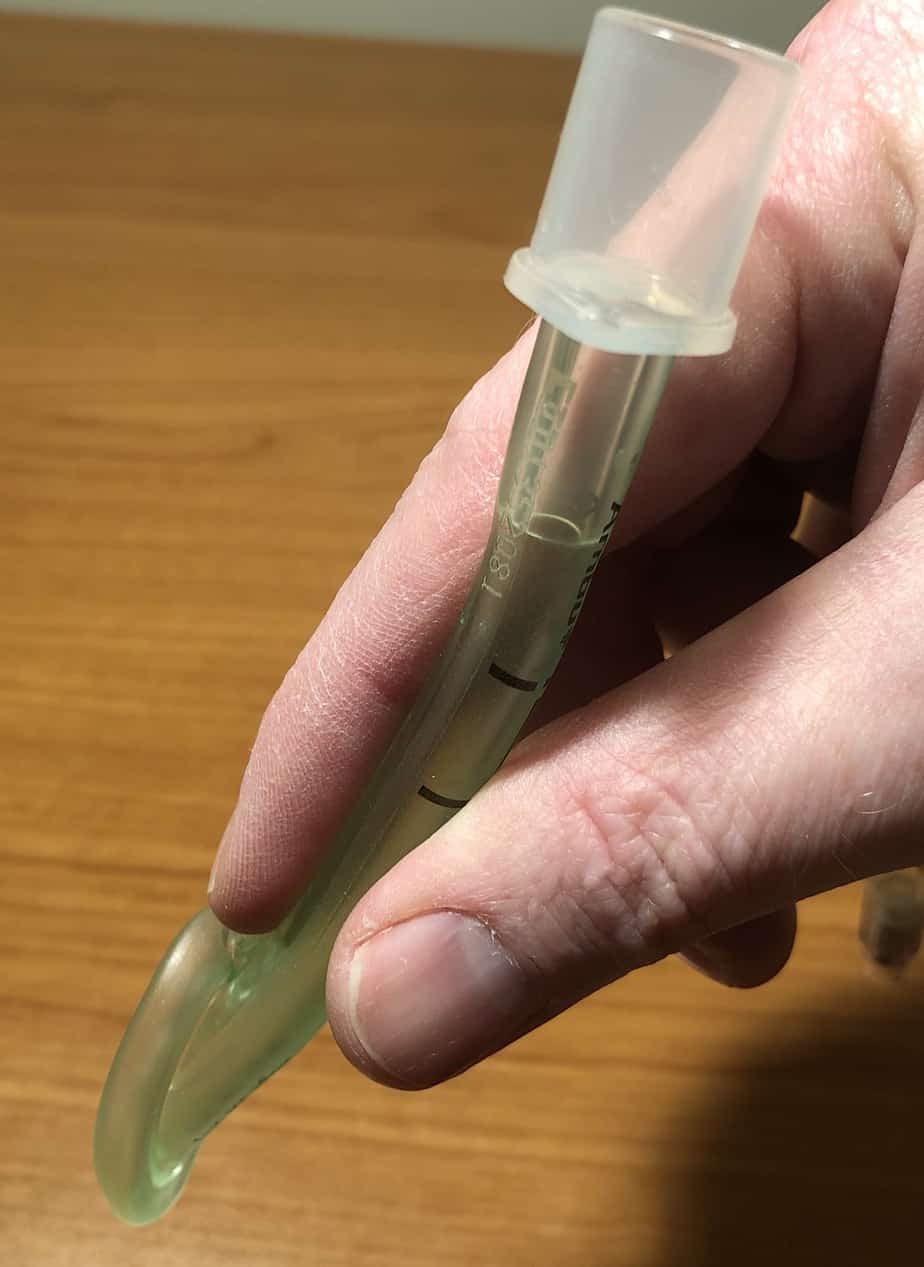
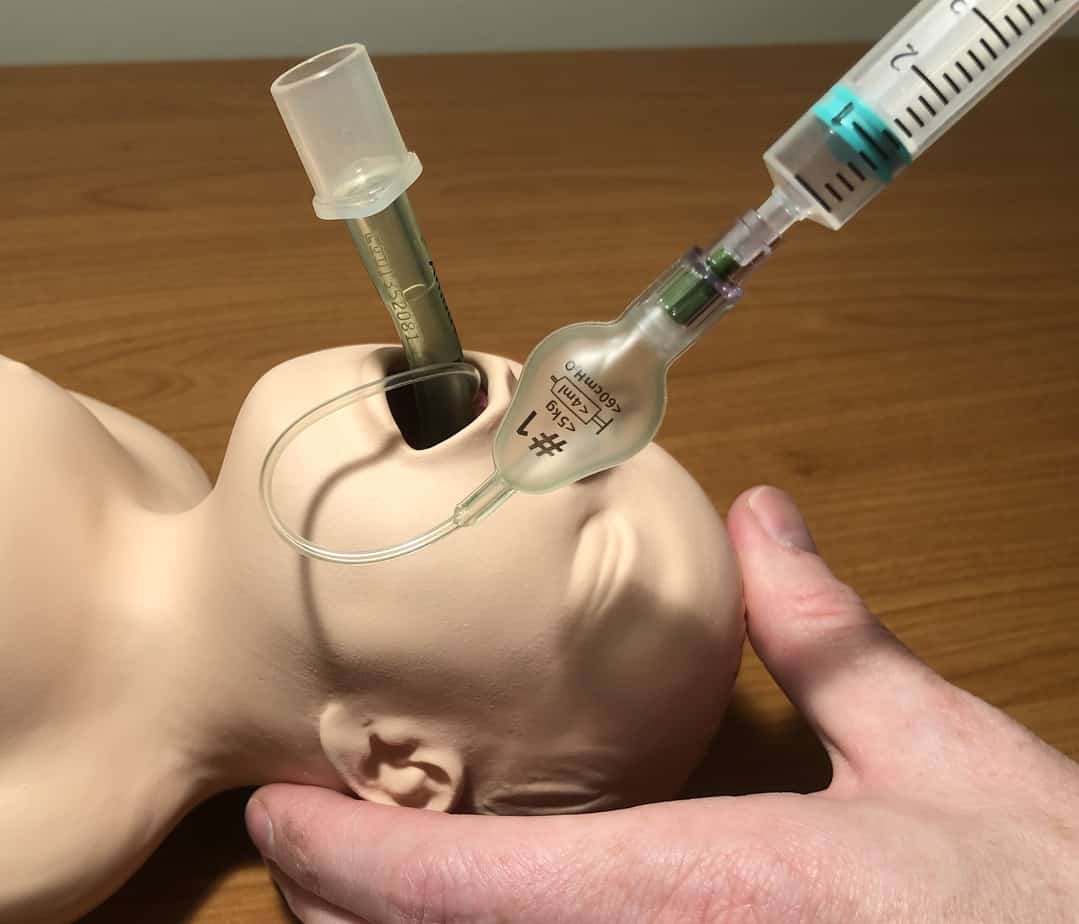
- The LMA is prepared by deflating the cuff, with the rim facing away from the mask aperture, with no folds near the tip. Some lubricant is applied to the dorsal surface to aid insertion.
- The LMA is held by the index finger and thumb of the right hand, such that the tip of the index finger is between the rim of the cuff and the shaft of the LMA. The LMA should be held initially so that its curvature matches that of the patient’s airway and the aperture is facing upwards (patient is supine).
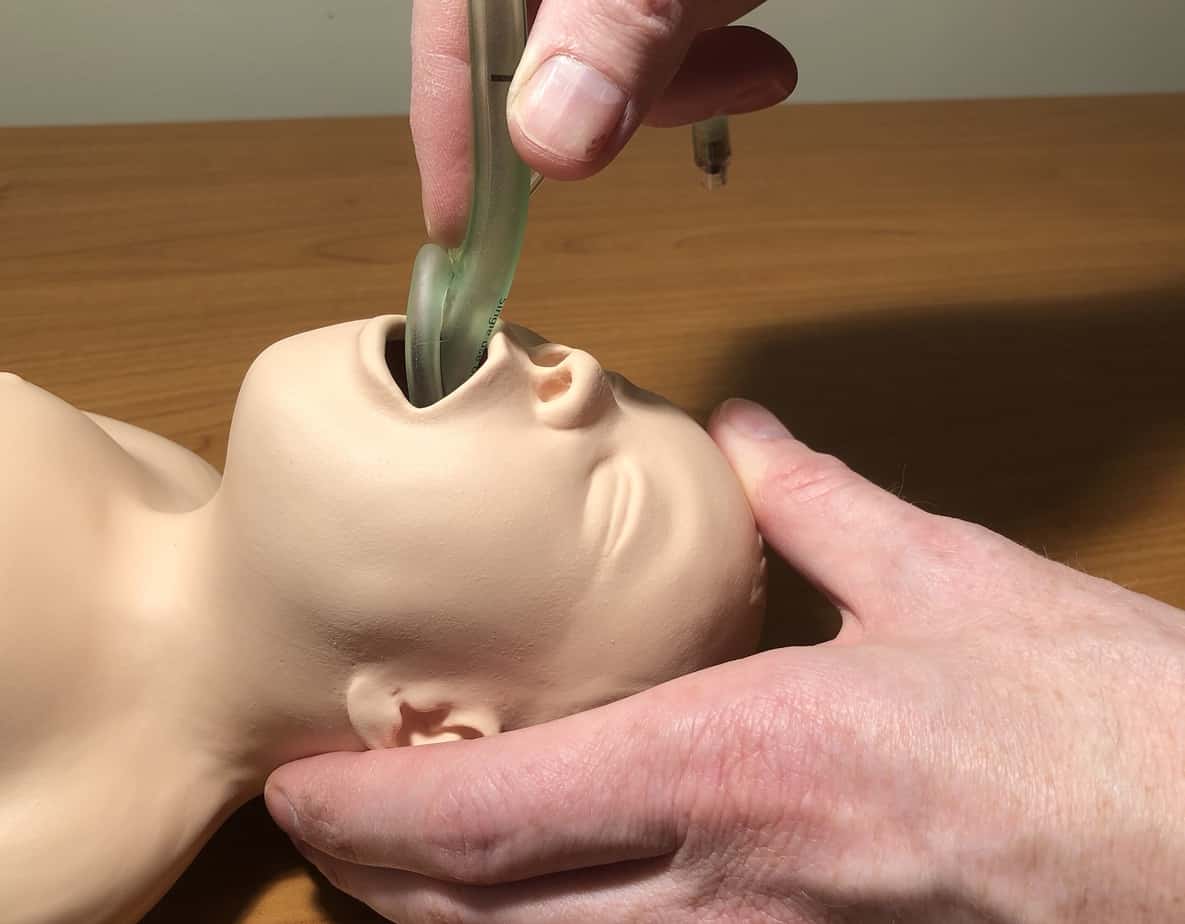
- With the head stabilised with the left hand, and in a similar position as that required for intubation, the LMA is inserted into the mouth, by pressing the tip against the hard palate and sliding it along the roof of the mouth between the tongue and the palate.

- This advancement of the LMA should be central, and continue with the thumb removed and index finger in place until the index finger can be inserted no further into the patient’s mouth. If necessary, the LMA can be carefully advanced further by pushing the tube, with the force continuing to be applied in the direction of the palate.

- Having let go of the LMA, the cuff should now be inflated to a pressure of approximately 20-30cmH2O, while not exceeding the recommended maximum inflation volume. It is likely that the LMA may move out slightly at this point, and this would indicate good positioning. [Note that the iGEL does not have a cuff].
Following these instructions carefully should normally cause the LMA to be positioned successfully. Common modifications to this technique, if the LMA is not positioning easily are:
- Ask an assistant to gently perform a jaw thrust / mouth opening manoeuvre while you are placing the LMA.
- Insert the LMA initially into the right hand side of the mouth and advance it as before, but with a rotational movement to bring the tip into the midline in the pharynx. (or other similar modification to the central insertion technique).
Rarely, a laryngoscope may be needed to assist in the placement of the LMA. Remember also to have the patient positioned well, in a similar way to that for preparing for endotracheal intubation.
If the LMA is still difficult to insert / fit, then consider changing size or type of LMA, as this may rectify the problem. Very occasionally, LMA insertion fails and the practitioner should have a plan to manage this situation also.
Trauma may occur during LMA placement, and this is usually associated with attempts to insert the LMA which are too forceful, and the LMA is not gliding into position as it is intended to do. If anything other than minor resistance is encountered, then pushing harder is not the answer; disimpacting the LMA and improving the positioning or trying a modified technique will normally allow for a smoother passage into the correct position.
Successful placement of the LMA
Successful placement of the LMA will be identified by finding that the spontaneously breathing patient is breathing easily through it, without noises or signs of an obstructed airway, and with a good ETCO2 trace and appropriate tidal volume. In a patient who is not breathing spontaneously, successful placement will be identified by easy ventilation through the LMA, without a leak (or a very minimal leak) during normal ventilation, and again, with a good ETCO2 trace. If these signs are not all present, the LMA may be misplaced and require removal and repositioning or substitution with another type of airway.
When successful placement has been achieved, the LMA should normally be secured in place with a tie or tapes, as with a tracheal tube, in order to mitigate against malposition / accidental removal. Situations change, and it is always necessary to monitor closely patients with LMAs in situ for signs that the airway is no longer as sufficient as it was, and appropriate action taken.
Videos demonstrating LMA insertion in children
Paediatric Anaesthetics: Chapter 2 – LMA insertion. World Federation of Societies of Anesthesiologists. Youtube. Copyright 2015 University Hospital Southampton, Reproduced under Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International
Paediatric Anaesthetics: Chapter 2 – IV induction igel. World Federation of Societies of Anesthesiologists. Youtube. Copyright 2015 University Hospital Southampton, Reproduced under Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International
![]()