Intubation in Special Circumstances
Listen to Lecture
This section will provide advice on how the standard technique should be modified and key points to remember when intubating children in four special circumstances.
1. Septic shock

Purpuric rash of meningococcal septicaemia. Reproduced with kind permission of Meningitis Research Foundation
Urgent semi-elective intubation and ventilation should be undertaken if there is ongoing signs of shock unresponsive to 40 ml/kg of fluid resuscitation or if there is airway obstruction/loss of protective airway reflexes at any stage, however cardiovascular resuscitation must occur before induction of anaesthesia.

Intubation and ventilation offers a number of advantages including providing significant support for the cardiovascular system/reducing oxygen demands, offering the ability to provide PEEP to combat inevitable pulmonary oedema and to facilitate insertion of central/arterial lines. However getting the haemodynamically unstable septic patient onto the ventilator without them arresting requires careful planning.
The airway should be supported with a face mask and bagging circuit in 100% oxygen with PEEP while preparation for intubation are made. Call for experienced help (Consultant Anaesthetist/Intensivist) and if time allows discuss your plan for induction of anaesthesia with the paediatric retrieval team.
Administer a further fluid bolus of 10 – 20 ml/kg of 0.9% saline or 4.5% albumin and start peripheral/intraosseous adrenaline at 0.1 mcg/kg/min (1 mg of adrenaline in 50 ml of 0.9% saline infused at 0.3 x weight in kg ml/hr = 0.1 mcg/kg/min) and titrate to effect. Ensure adrenaline has reached patient through the line prior to induction of anaesthesia. Alternatively if the patient has already been started on dopamine prepare ‘Push Dose’ adrenaline (1 in 100,000) by diluting 1 ml of adrenaline 1 in 10,000 with 9 ml of 0.9% saline to be used to treat any cardiovascular instability on induction.
Brief all team members of the high risk of cardiac arrest on induction and have resuscitation drugs prepared. In the absence of an arterial line ensure the non-invasive blood pressure is cycling every minute and allocate a member of staff to keep a finger on the pulse.
Propofol, thiopentone and midazolam should not be used for induction in the haemodynamically unstable septic patient. Although ketamine is the safest induction agent, due to exhaustion of endogenous catecholamines, cardiovascular instability should still be expected with its use in this situation. Modified RSI with ketamine (reduce dose to 0.5 – 1 mg/kg) and rocuronium 1 mg/kg by most experienced operator. Expect the effects of the ketamine to take longer than usual to become evident due to impaired circulation time and avoid the temptation to give more too quickly.
Consider prophylactic atropine (particularly in infants or if you have elected to use suxamethonium).
Use a cuffed oral tube regardless of age and don’t change to a nasal tube due to likely coagulopathy and risk of bleeding.
2. Duct dependant congential heart disease

Cyanotic Neonate. Author: Jules Atkins, RM. Supplied by: Brandi Catt. Wikipedia. Copyrighted free use, via Wikimedia Commons
Due to their underlying heart disease these babies are unlikely to tolerate intubation well and cardiovascular instability on induction of anaesthesia should be expected and prepared for similarly to the septic patient (see above). If the patient is not currently shocked, but has the potential to become shocked, administration of a fluid bolus prior to induction of anaesthesia and preparation of push dose adrenaline may be preferred to routinely starting an adrenaline infusion (however the risks and benefits of each intervention must be considered on a case by case basis by an experienced clinician). If you do decide to start an adrenaline infusion you may wish to start at a lower dose than with the septic patient e.g. 0.05 mcg/kg/min (depending on the individual patients haemodynamics) with the aim of providing inotropy without increasing the afterload on the heart.
In addition the oxygen concentration used for pre-oxygenation should be limited to 30 – 40% at most, targeting peripheral oxygen saturations of 75 – 85%, as excessive oxygen may cause the ductus arteriosus to close.

Extra caution must be taken in babies with univentricular anatomy e.g. hypoplastic left heart syndrome, where either the administration of excessive oxygen (SpO2 > 85%) or hyperventilation (causing ↓CO2) will both lead to pulmonary vasodilation and excessive pulmonary blood flow at the expense of reducing blood flow to the systemic circulation putting the baby at risk of circulatory collapse and ultimately cardiac arrest.
3. Unfasted patient
Traditional teaching dictates that emergency intubation of the unfasted or critically ill patient (where gastric emptying may be unreliable) should be done following a rapid sequence induction (RSI) of anaesthesia. This involves preoxygenation, application of cricoid pressure, administration of a pre-calculated dose of an induction agent followed immediately by a fast acting muscle relaxant. During the apnoea period (while waiting for the muscle relaxant to take effect) face mask ventilation is not administered and once the muscle relaxant has taken effect the patient is intubated. Cricoid pressure is only removed after correct positioning of the endotracheal tube has been confirmed with capnography and the endotracheal tube cuff has been inflated. The following video demonstrates how to perform a RSI.
Paediatric Anaesthetics: Chapter 3 – Intubation rsi child. World Federation of Societies of Anesthesiologists. Youtube. Copyright 2015 University Hospital Southampton, Reproduced under Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International
The main advantage of the RSI is to reduce the risk of aspiration in high risk patients. When performing a RSI you are taking a gamble that you will be able to intubate the patient quickly and without difficulty, therefore it should not be performed in patients with an anticipated difficult airway (the risk and complications of failed intubation outweigh the risks of aspiration).
Cricoid pressure is posterior pressure applied to the cricoid cartilage designed to occlude the oesophagus and prevent regurgitation and aspiration. While regarded as a standard of care during rapid sequence induction for many years this is actually based on weak evidence as the video below demonstrates.
The use of cricoid pressure is not without problems, as poorly applied cricoid pressure can impair the view and prevent intubation.
Poorly applied cricoid pressure deviating airway to right hand side during Airtraq intubation of 2kg neonate with copious secretions
Another problems with this technique is that as the patient does not receive face mask ventilation during the apnoea period, meaning that patients with lung pathology (even with adequate preoxygenation) are at risk of critical hypoxia during the process. This may also cause problems in patients with normal lungs as during the apnoea period oxygen can still move from the reservoir in the lungs by diffusion, however elimination of CO2 requires ventilation. While most patients will tolerate a brief period of hypercapnia without problems, certain groups of patients won’t e.g. traumatic brain injury patients where it may elevate intracranial pressure or patients who already have a significant metabolic acidosis where even a short interruption in ventilation (loss of compensatory Kussmaul breathing) will cause the pH to plummet to dangerously low levels.
As it is not without risk a rapid sequence induction should only be performed when the advantages of doing so outweigh the disadvantages. This is rarely the case during the emergency intubation of the critically ill child outside of the anaesthetic room. The main factors limiting use of this technique in these children is the smaller functional residual capacity of the lungs and higher demand for oxygen, meaning that even with optimal preoxygenation, critical desaturation is highly likely during the apnoea period. The smaller the patient the more noticeable this is and the critically ill neonate is highly likely to desaturate during endotracheal intubation (even with slick intubation following face mask ventilation), so trying to preform a RSI in this patient population is highly likely to be met with complications.
Although performing a classical rapid sequence induction is not in the best interest of most critically ill children, they are still at risk of regurgitation and aspiration during emergency endotracheal intubation and steps to prevent this need to be taken.
Firstly consideration should be given to delaying intubation until the child is adequately fasted. While this may be an option for some patients requiring semi-elective intubation e.g. to facilitate a procedure, delaying emergency intubation is unlikely to be appropriate and as gastric emptying in the critically ill child is unreliable doing so will not eliminate the risk of aspiration.
If possible the child should be kept in a slight head up position during the intubation, rather than lying flat, as this will not only reduce the risk of regurgitation but may also improve oxygenation. As it has already been mentioned, even if the child has been adequately fasted there is no guarantee that the stomach is empty. Therefore it makes sense that if there is a nasogastric tube in situ, that gastric content should be aspirated prior to induction of anaesthesia. If the child doesn’t have a nasogastric tube in situ consideration should be given to inserting one after weighing up the risks (inducing vomiting, respiratory deterioration secondary to increased agitation) and benefits (aspiration of gastric content prior to induction and of air during face mask ventilation) on a case by case basis. An alternative is to insert the tube after induction of anaesthesia (gag reflex suppressed), but before face mask ventilation causes distention the stomach.
Face mask ventilation should be gentle and a balance needs to be struck between inflating the lungs while trying not to inflate the stomach. However this becomes much less of a problem if a member of the team is allocated to continuously aspirate the nasogastric tube during face mask ventilation. The decision of whether to use cricoid pressure should be made after weighing up the evidence of risk verses harm and after considering the individual patient’s circumstances.
4. Unanaesthetised patient
Prior to intubation the patient should receive an induction agent (causes unconsciousness so that the patient is unaware of the procedure and the physiological response to the stimulus of laryngoscopy is reduced) and a muscle relaxant (relaxes the muscle tone and abolishes the protective airway reflexes allowing laryngoscopy and causes the vocal cords to relax in the open position facilitating passage of the endotracheal tube). Administration of these medications prior to intubation is standard anaesthetic practice and while I don’t recommend trying to intubate without them (they make intubation easier and safer), as intubation of babies without any medications occurs routinely in delivery suite and intubation following the administration of only an induction agent is standard practice in many neonatal units, I feel it is important to provide an approach for dealing with a life threatening complication that can occur as a consequence of this approach.
Laryngospasm is spasmodic closure of vocal cords in response to a stimulus which can be local (instrumentation of the airway) or systemic (painful stimulus elsewhere) normally occurring in a light plain of anaesthesia. If complete vocal cord closure occurs both face mask ventilation and endotracheal intubation may be impossible and unless promptly recognised and appropriate treatment given, life threatening hypoxia will quickly occur.
Video demonstrating laryngospasm occurring during attempted intubation of a patient who is sedated but not paralysed (due to them having a known difficult airway)
Treatment of laryngospasm involves providing oxygen with PEEP while anaesthesia is quickly deepened (e.g. using propofol) or by administration or a fast acting muscle relaxant e.g. suxamethonium. If you intubate without giving muscle relaxant you must have plan for how you will deal with laryngospasm. For those working in neonatology the most accessible and familiar drug is likely to be suxamethonium.
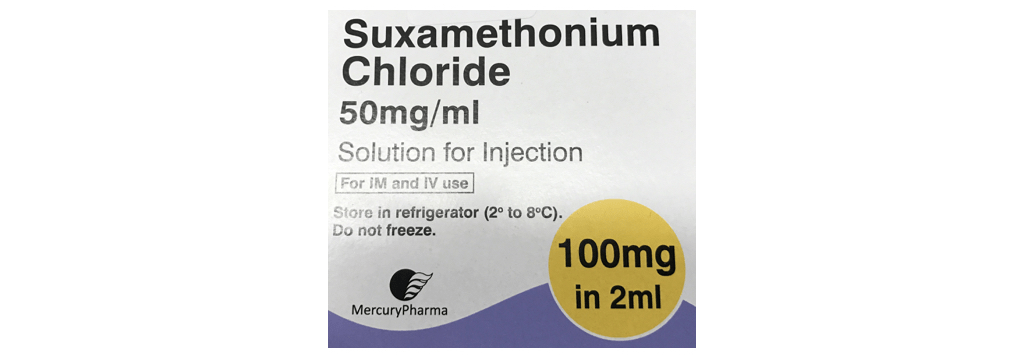
Suxamethonium is normally given to neonates in a dose of 2 mg/kg to facilitate endotracheal intubation, where it acts in approximately 30 seconds. It can also be given by intramuscular injection in a dose of 4mg/kg where it acts in around 2 minutes. As providing treatment for laryngospasm is time critical you need to have memorised these doses and have a plan for how you will reconstitute and administer suxamethonium in an emergency that will work for the range of weights of patients you will encounter. Suxamethonium comes in a concentration of 50 mg/ml, which doesn’t lend itself to easy conversion from a dose in mg to a volume in ml in your head and also means that further dilution is needed to allow accurate administration of the small doses needed for neonates.
One example of a plan for doing this is outlined below. You don’t have to use this method, but you must have a solution that you can recall from memory when needed (you will likely be managing the airway and may need to instruct someone else on preparing and giving the suxamethonium) and this must also include a plan for when IV access is not available.
Suxamethonium dosing for laryngospasm
Dilute 0.4 ml of Suxamethonium (50 mg/ml) with 0.6 ml of 0.9% saline to make a solution of concentration 20 mg/ml. Administer 0.1 ml/kg (2 mg/kg) of the reconstituted (20 mg/ml) solution by intravenous or intraosseous injection (easy to remember as same volume of adrenaline for a cardiac arrest).
If intravenous access is not available double the dose to 0.2 ml/kg (4 mg/kg) of the reconstituted (20 mg/ml) solution and give by intramuscular injection (ensure the needle you are using for injection has been primed with the reconstituted solution).
![]()