Listen to the Podcast
Initial Management
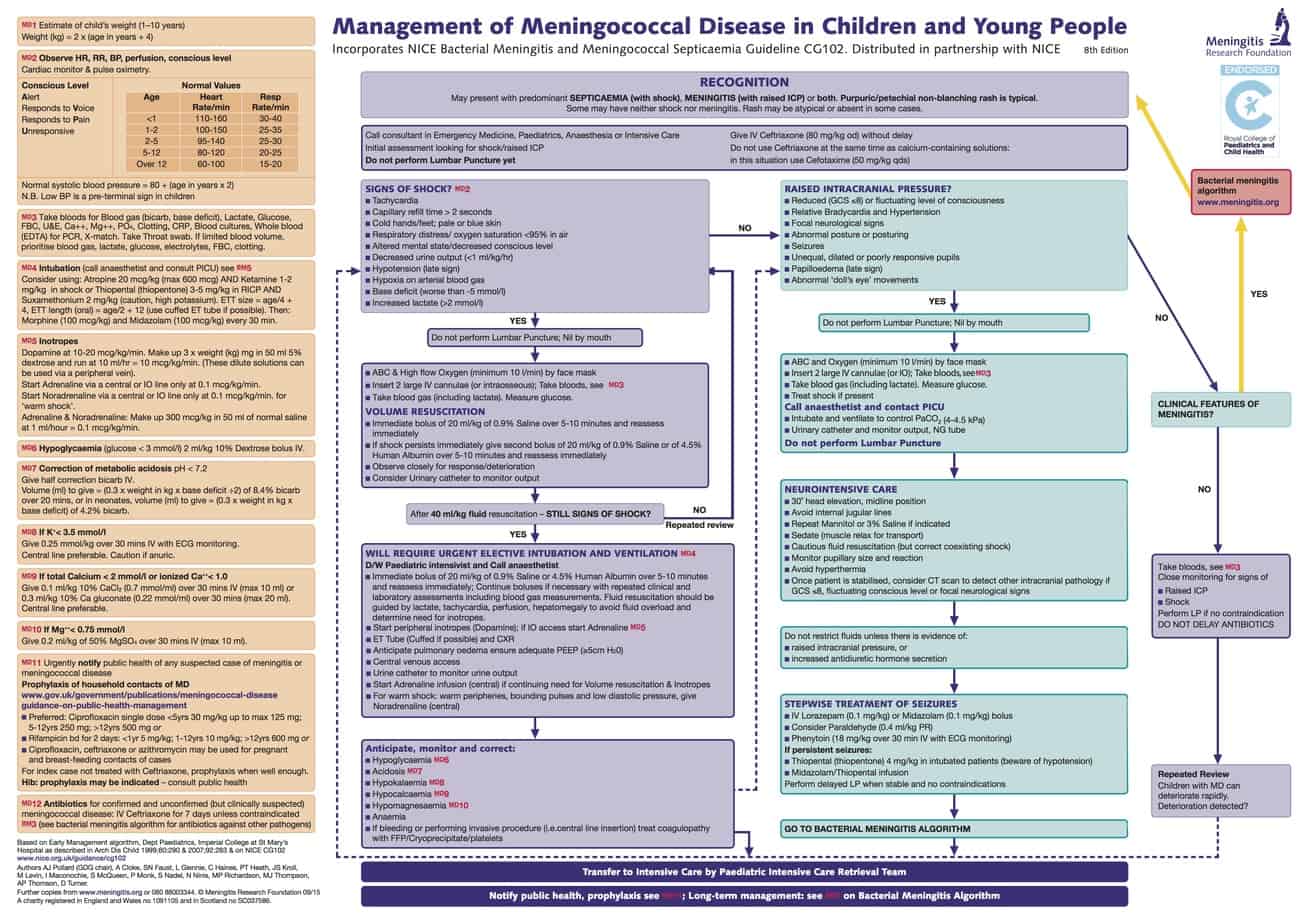
Management of Meningococcal Disease in children and Young People. Meningitis Research Foundation, 2015. Reproduced with kind permission of MRF
Airway
Urgent semi-elective intubation and ventilation should be undertaken if there is ongoing signs of shock unresponsive to 40 ml/kg of fluid resuscitation or if there is airway obstruction/loss of protective airway reflexes at any stage (cardiovascular resuscitation should occur before induction of anaesthesia).
Intubation and ventilation offers a number of advantages including providing significant support for the cardiovascular system/reducing oxygen demands, offering the ability to provide PEEP to combat inevitable pulmonary oedema and to facilitate insertion of central/arterial lines. However getting the haemodynamically unstable septic patient onto the ventilator without them arresting requires careful planning.
Support the airway with mask and anaesthetic bagging circuit in 100% oxygen with PEEP while preparation for intubation are made. Call for experienced help (Consultant Anaesthetist/Intensivist) and if time allow discuss your plan for induction of anaesthesia with the retrieval team.
Administer a further fluid bolus of 10 – 20 ml/kg of 0.9% saline or 4.5% albumin and start peripheral/intraosseous adrenaline at 0.1 mcg/kg/min (1 mg of adrenaline in 50 ml of 0.9% saline infused at 0.3 x weight in kg ml/hr = 0.1 mcg/kg/min) and titrate to effect – Ensure adrenaline has reached patient through the line prior to induction of anaesthesia. Alternatively if the patient has already been started on dopamine prepare ‘Push Dose’ adrenaline (1 in 100,000) by diluting 1 ml of adrenaline 1 in 10,000 with 9 ml of 0.9% saline to be used to treat any cardiovascular instability on induction.
Brief all team members of the high risk of cardiac arrest on induction and have resuscitation drugs prepared. In the absence of an arterial line ensure the non-invasive blood pressure is cycling every minute and allocate a member of staff to keep a finger on the pulse.
Propofol, thiopentone and midazolam should not be used for induction in the haemodynamically unstable septic patient. Although ketamine is the safest induction agent, due to exhaustion of endogenous catecholamines, cardiovascular instability should still be expected with its use in this situation. RSI with ketamine (reduce dose to 0.5 – 1 mg/kg) and rocuronium 1 mg/kg by most experienced operator. Expect the effects of the ketamine to take longer than usual to become evident due to impaired circulation time and avoid the temptation to give more too quickly. Consider prophylactic atropine (particularly in infants or if you have elected to use suxamethonium).
Use a cuffed oral tube regardless of age and don’t change to a nasal tube due to likely coagulopathy and risk of bleeding.
Breathing
Routine settings on ventilator i.e I:E ratio 1:2. Ti < 1 year = 0.6 – 0.8 seconds, 1-5 years = 0.8 – 1 seconds, 5-12 years = 1-1.2 seconds, >12years = 1.2-1.5 seconds and adjust depending on blood gases.
Start with a PEEP of 5 cmH2O, however this may need to be increased as pulmonary oedema develops (remember using more PEEP than required with reduce venous return). Adjust the FiO2 and PEEP to target SpO2 of 100% in an attempt to maximise oxygen delivery to the tissues.
A peak pressure of around 20 – 25 cmH2O or tidal volume of 6-8 ml/kg is a reasonable starting point and adjust depending of chest movement and blood gases.
Target a PaCO2 of 4.5 – 5 kPa and PaO2 > 10 kPa if there is any suspicion of raised intracranial pressure. Continuously monitor end tidal CO2 and correlate this with PaCO2.
Chest radiograph following intubation for endotracheal tube position.
Circulation
Insert an ultrasound guided central venous line (femoral site preferred) and a peripheral arterial line. A short large bore peripheral cannula is useful as a volume line.
Continuously monitor ECG, CVP and invasive arterial blood pressure. Monitor urine output hourly and perform paired arterial/venous blood gases for lactate and central venous oxygen saturation (ScvO2) every 30 – 60 minutes initially.
Target normalisation of the heart rate, CVP ≥ 8 cmH2O, normal BP for age, lactate clearance, ScvO2 ≥ 70%, central capillary refill time <2 secs, normal pulse volume with no differential between peripheral and central pulses, warm peripheries and urine output ≥ 1 ml/kg/hr. NB Blood pressure targets are often defined in terms of mean arterial pressure (MAP). It is however also important to consider pulse pressure to determine the state of the systemic vascular resistance and guide choice of vasoactive drugs i.e. low systemic vascular resistance = wide pulse pressure with diastolic BP less than half the systolic pressure, and high systemic vascular resistance = narrow pulse pressure.
Consider giving further fluid boluses in 10ml/kg aliquots if the above targets are not met and CVP < 8 cmH2O or if there is a significant swing on arterial tracing with respiration. Evidence that the fluid bolus would be helpful prior to its administration can be gained by either applying sustained pressure over the liver or passive leg raising (raise the foot of the bed). Both manoeuvres with increase preload to the heart without actually expanding the circulating volume, so if this causes the blood pressure to increase and heart rate to decrease it suggests a further fluid bolus would be helpful.
If despite adequate fluid resuscitation and titration of adrenaline for cold shock and noradrenaline for warm shock, the haemodynamic targets are not being met (particularly if lactate is not clearing or if ScvO2 remains < 70%) discuss further management strategy with retrieval team. Packed red cells should be transfused if haemoglobin is < 100 g/L and low dose hydrocortisone 1 mg/kg should be administered in the setting of fluid and inotrope resistant shock. Further management will depend in which of the following three categories the patient falls into:
- Cold shock with normal/high blood pressure – If after titrating fluid, adrenaline and packed red cell transfusion the lactate is not clearing and ScvO2 remains < 70%, start milrinone at 0.3 mcg/kg/min (omit loading dose). As the patient dilates additional filling will be required.
- Cold shock with low blood pressure – If after titrating fluid and adrenaline the patient remains hypotensive titrate noradrenaline. If despite this the lactate is not clearing and ScvO2 < 70% consider adding either dobutamine or milrinone (no loading dose).
- Warm shock with low blood pressure – If after titrating fluid and noradrenaline the patient remains hypotensive start vasopressin at 0.0003 units/kg/min. If despite this the lactate is not clearing and ScvO2 < 70%, commence low dose adrenaline if not already started.
Algorithm for time-sensitive, goal-directed stepwise management of hemodynamic support in infants and children, American College of Critical Care Medicine, 2017. Reproduced with kind permission of the Society of Critical Care Medicine.
Disability
Keep the patient sedated with morphine (10 – 60 mcg/kg/hr), midazolam (1 – 4 mcg/ kg/min) and muscle relaxed to reduce oxygen demands.
If meningitis is also present the patient is at risk of cerebral oedema which will be made worse with the volume resuscitation. Observe for signs of raised intracranial pressure (GCS ≤8 or fluctuating level of consciousness, relative bradycardia and hypertension, focal neurological signs, abnormal posture or posturing, seizures, unequal, dilated or poorly responsive pupils, papilloedema, abnormal ‘doll’s eye’ movements) and if present administer 3ml/kg of 3% hypertonic saline over 15 minutes and ensure neuroprotective measures (see raised ICP section) are adhered to.
Monitor blood glucose – hyperglycaemia secondary to the stress response is common, but insulin sliding scale is not normally required outside the intensive care environment.
Sepsis
Early appropriate antibiotics should be given as soon as possible and must be given within 1 hour of presentation. Ideally take blood culture prior to the administration of antibiotics, provided this doesn’t significantly delay their administration.
For community acquired sepsis with unknown source in an immunocompetent patient administer:
Age <3/12 – cefotaxime 50 mg/kg and amoxicillin 50 mg/kg
Age ≥ 3/12 – cefotaxime 50 mg/kg or ceftriaxone 80 mg/kg
If erythroderma, diarrhoea or other features of toxic shock are present add clindamycin 10 mg/kg and consider administration of normal immunoglobulin (2g/kg).
For hospital acquired sepsis administer 40 mg/kg of meropenem +/- 15 mg/kg of vancomycin (indwelling central line or known MRSA).
Consider previous cultures/colonisation.
Consider need for antiviral and anti-fungal treatment in immunocompromised patients. Neonates with severe sepsis should be treated with aciclovir to cover congenital herpes simplex infection (particularly if there are risk factors or liver disfunction).
Consider whether source control is needed (debridement, drainage of collections or remove of infected material)
A lumbar puncture is contraindicated in the acute phase of septic shock and MUST NOT be performed.
Aim for normothermia to reduce metabolic demands and oxygen requirements. Treat elevated temperature with antipyretics and consider active cooling.
Renal
Restrict intravenous fluids to 80% maintenance and use isotonic fluids due to risk of SIADH e.g. 0.9% saline and 5% dextrose +/- added potassium depending on serum potassium.
Catheterise the bladder and monitor urine output (aim ≥ 1ml/kg/hr).
Gastrointestinal
Keep nil by mouth.
Insert and aspirate nasogastric tube (to remove any swallowed air splinting the diaphragm), then leave on free drainage.
Labs & Electrolytes
Routinely check FBP, clotting, cross-match, U&E, Ca, Mg, PO4, LFTs, glucose, CRP, blood gas, lactate, blood cultures and whole blood (EDTA) for meningococcal PCR.
Transfuse packed red cells (15 ml/kg) if Hb < 100 g/L, fresh frozen plasma (10 ml/kg) for DIC, cryoprecipitate (5 ml/kg) if fibrinogen < 1g/L and platelets (10 ml/kg) if platelets < 50×109.
Keep Ca > 2 mmol/L (iCa > 1 mmol/L), K > 3.5 mmol/L and Mg > 0.75 mmol/L. Half correct base deficit using bicarbonate if pH < 7.2 despite fluid resuscitation – see Meningitis Research Foundation algorithm for instructions. NB Hypocalcaemia and acidosis are common causes of inotrope failure in the septic patient and should be corrected.
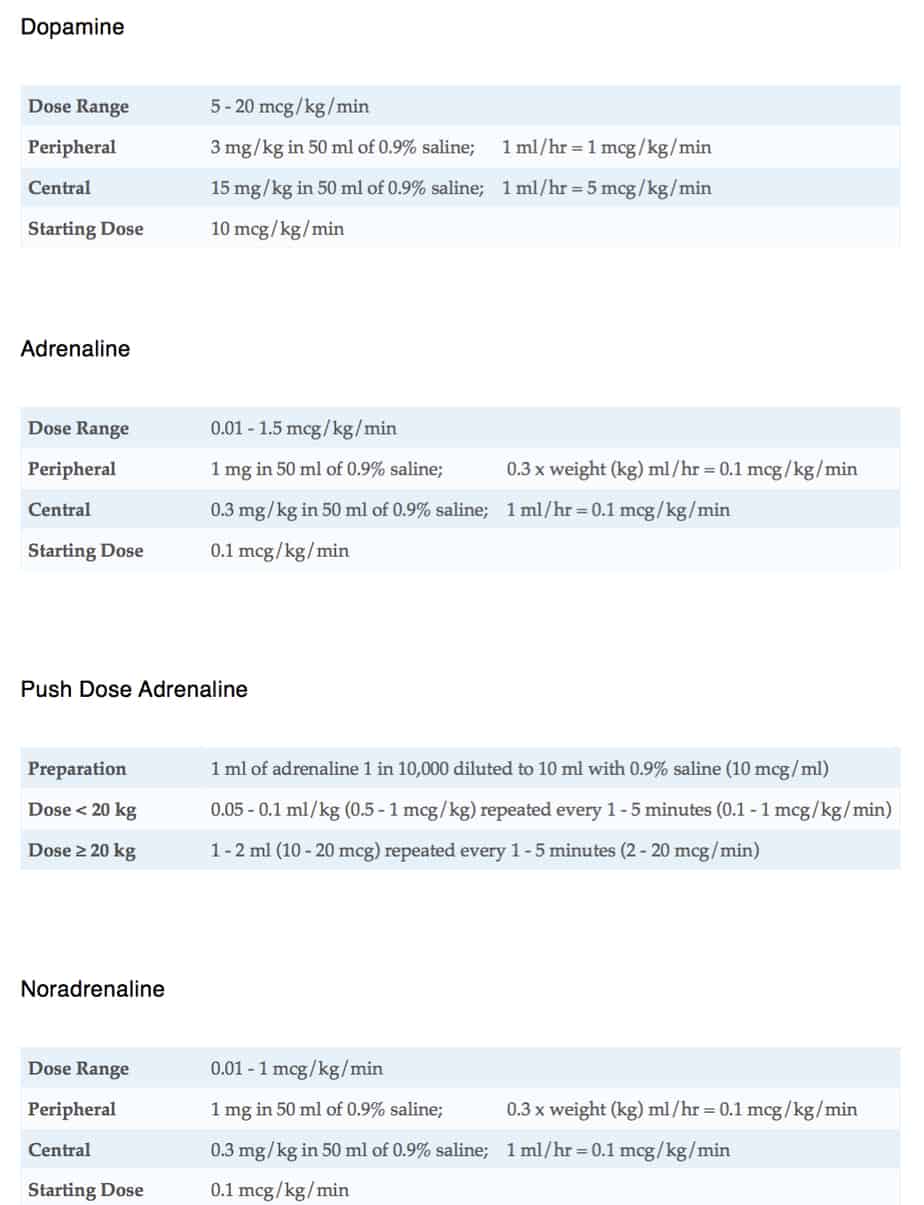
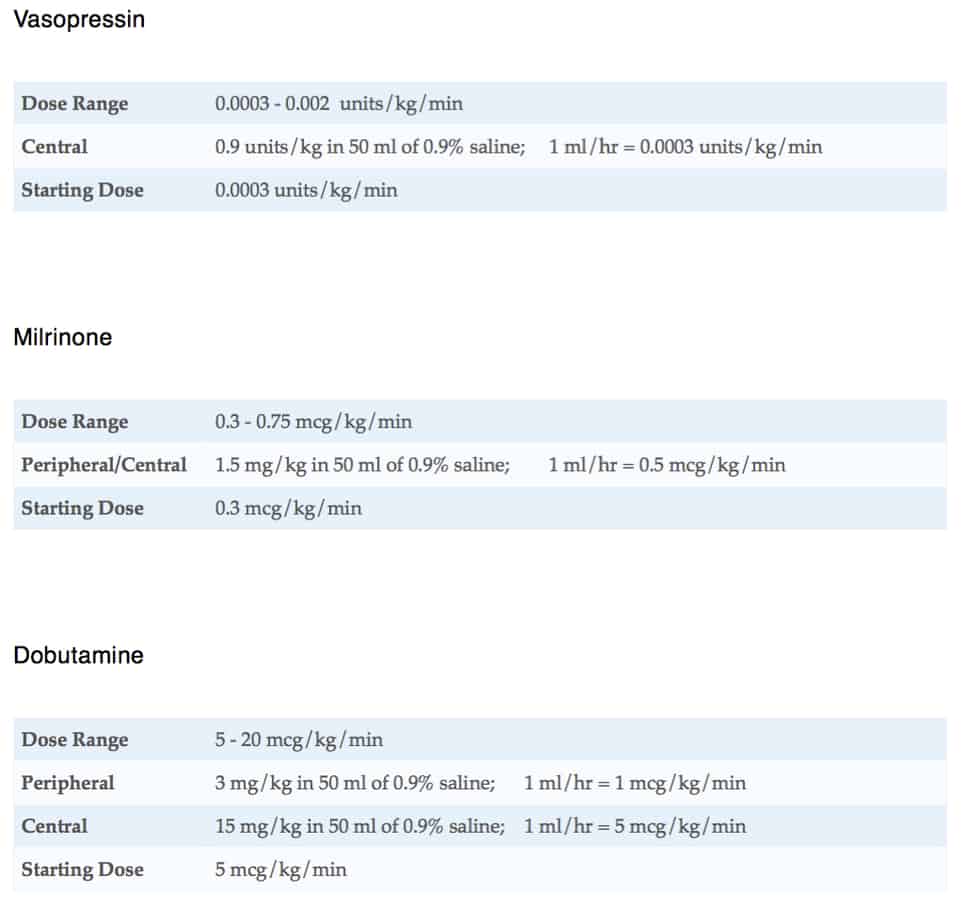
Drugs & Infusions
Additional Information
If the lactate is not clearing or the patient shows ongoing signs of shock discuss ongoing management with the retrieval team – don’t just turn up the existing vasoactive drugs as this can make things worse.
Consider if you have the correct diagnosis – in the ‘septic neonate’ congenital heart disease and an inherited metabolic disorder must be excluded (see collapsed neonate section).
For all children consider the following differential diagnosis (which can coexist with sepsis) – tension pneumothorax, pericardial effusion, intussusception/volvulus, myocarditis, DKA, toxin ingestion anaphylaxis, arrhythmia, haemorrhage, myocardial infarction, pulmonary embolism, adrenal insufficiency, hypothyroidism, metabolic disorder and intra-abdominal pressure > 12 mmHg.
Rescue treatments for refractory septic shock include plasma exchange (removes inflammatory mediators) and ECLS.
![]()


Thanks for a great podcast. May I ask a couple of questions?
Do you tend to use peripheral Adrenaline as your first choice in initial stabilisation? All the guidelines seem to suggest dopamine, but all adult intensivists, who generally resuscitate the sick children in DGHs the UK, are much more used to using adrenaline!
Do you give stress ulcer prophylaxis or DVT prophylaxis?
Many thanks
again.
Hi Mat, glad you found it useful. In my experience adrenaline is a superior drug to dopamine (it has worked on numerous occasions when dopamine has failed) it is easier to make up and is in every resus trolley. It is just as safe to give peripherally or via IO. The actual evidence that it is better is not as strong as my opinion, but there is some evidence in favour of it over dopamine and this was deemed strong enough for the American colleague of critical care medicine to recommend it as the first line vasoactive drug in septic shock in kids (see their algorithm https://journals.lww.com/ccmjournal/Fulltext/2017/06000/American_College_of_Critical_Care_Medicine.18.aspx). I think the other UK guidelines will follow and for me it makes sense to start with the drug most likely to work. I don’t use stress ulcer prophylaxis in all critically ill children, but do so in certain circumstances based on risk factors. I normally provide DVT prophylaxis in post pubertal patients or where there is other risk factors, but this is most often with TED stockings and flowtrons rather than heparin.